Butorphanol: So sticky it sucks
Butorphanol is an agonist-antagonist opioid that has a long history in veterinary medicine for “pain relief” and sedation. Typical analgesia of butorphanol in animals is only 30-150min- other reviews suggest only 60min in dogs and 90min in cats.
https://www.sciencedirect.com/science/article/pii/B978032304679410022X
https://www.sciencedirect.com/science/article/pii/B9781416048893000267
https://journals.sagepub.com/doi/abs/10.3181/00379727-197-43258
Sedation- Butorphanol’s ability to produce sedation compared to other opioids is due to its affinity on the Kappa opioid receptors. Peak analgesic activity- 30-60min.
Agonist effects of opioid receptors:
Mu- Analgesia (moderate), respiratory depression, bradycardia, euphoria, pruritis, GI motility, miosis, immune response, addiction
Kappa- Analgesia (moderate- bone pain-short duration), sedation
https://www.jpain.org/article/S1526- 5900(18)30025-7/fulltext
Delta- Analgesia (severe), modulation of Mu receptor activity, GI motility
OLR (NOR)(ZOR)- Analgesia (moderate), immune response, modulation of TRPV receptors, regulate developmental events https://www.ncbi.nlm.nih.gov/books/NBK546642/
For acute and chronic pain: Except for a handful of procedures there is little to no room for butorphanol when entering a body cavity, orthopedic or invasive dental procedures. While there is some analgesia during the procedure the fact of the matter is that acute pain is not addressed outside of that narrow window butorphanol offers, even with multimodal approaches. When using a multimodal approach with drugs that also have analgesic properties like ketamine, dexmedetomidine, they do not offer long term or in some cases adequate analgesic coverage- and could potentially inhibit better analgesia when full mu opioids are introduced (see nuance section). It’s also important to remember sedation is not always synonymous with analgesia!
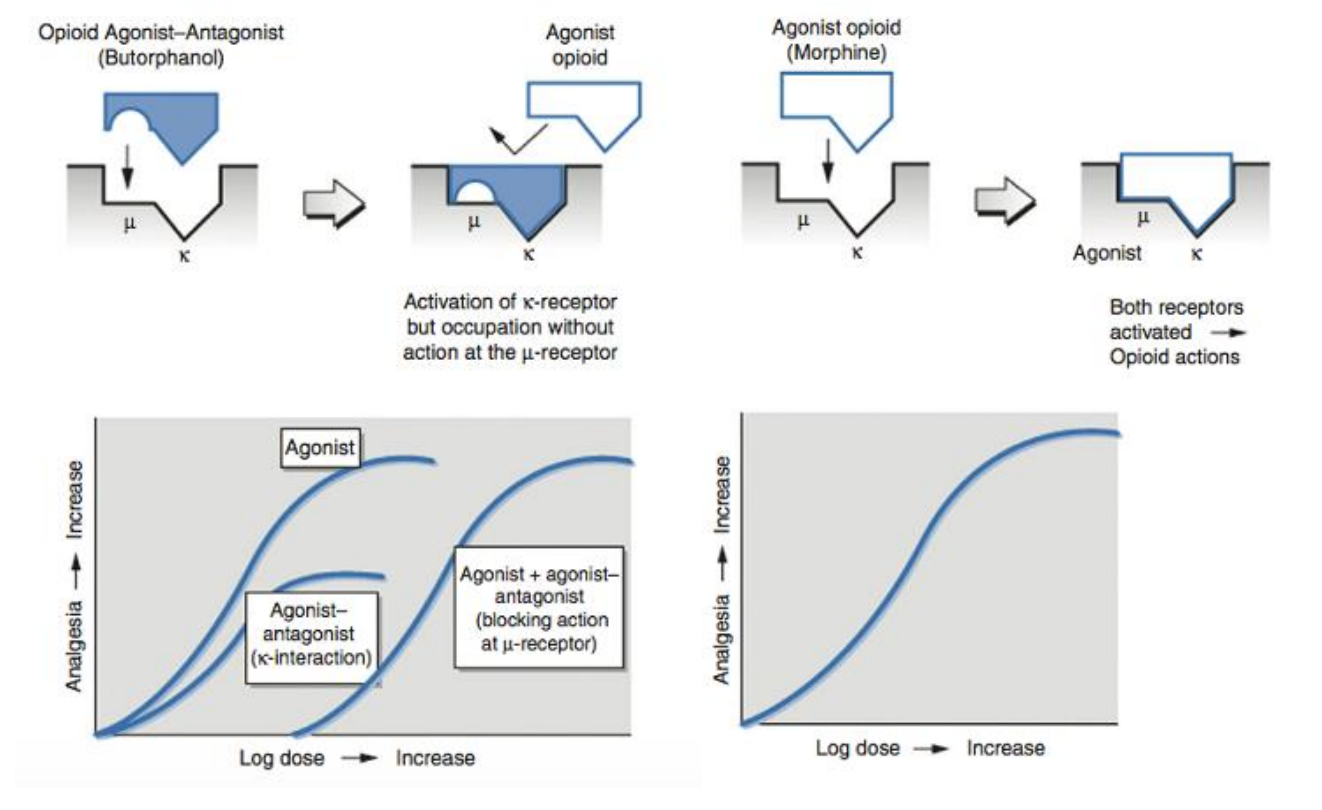
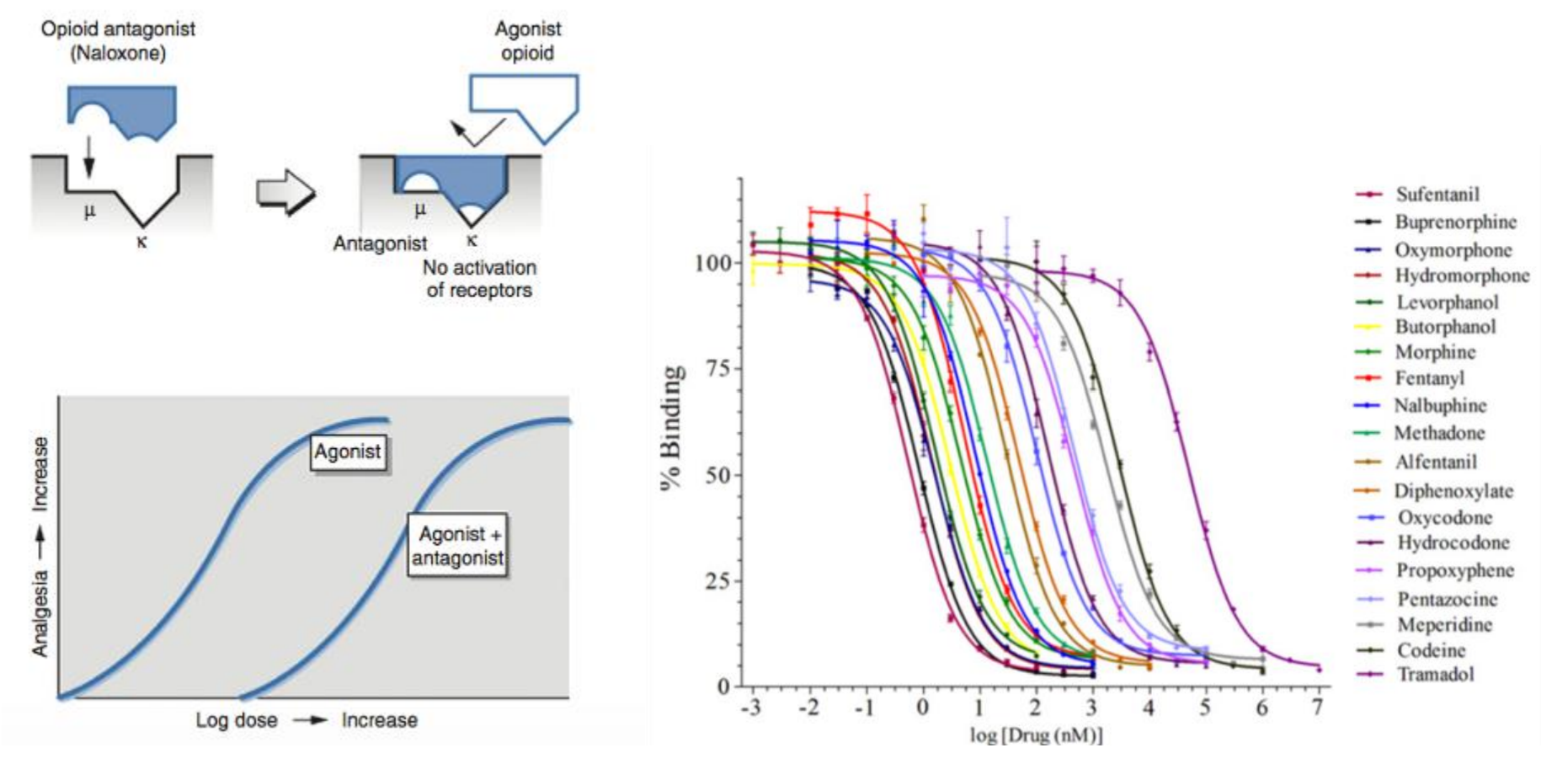
Nuances of using butorphanol: Mixing with other opioids within a short period of time is fraught with nuance. Here are the main concepts to remember. Butorphanol’s affinity to the opioid receptor (mu and kappa) compared to other opioids except for buprenorphine, (+/-)hydromorphone and sufentanil is strong. Butorphanol’s highest affinity is to the kappa receptor. https://pubmed.ncbi.nlm.nih.gov/32701545/ This means when using a large dose of butorphanol one can saturate all the available opioid receptors that then would block other, more useful opioids- but not render them useless per se. Regardless, not an awesome practice to get sucked into.
However, depending on the dose used it is conceivable that one can mix butorphanol and another opioid like hydromorphone- but dose is EVERYTHING! One can give a low dose of butorphanol (0.01 mg/kg- note that dose!) given its low intrinsic activity and only expect ~5% decrease in efficacy of other full mu opioids.
https://www.sciencedirect.com/science/article/pii/B978032308935700015
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1532-950X.1994.tb00447.x
Doses exceeding 0.1mg/kg will have antagonistic effects- a good option for reversal of a dysphoric animal without negating all analgesia for a short period of time.
https://pubmed.ncbi.nlm.nih.gov/1785725/
Successful mixing of opioids is not only dependent on the dose of the opioids used and the time between administration, but also the number of static and proliferative opioid receptors available.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3371376/
https://www.nature.com/articles/1395551
The more receptors there are the more room for various opioids to find binding sites (orthosteric binding sites).
The problem with mixing and the general view from many pain specialists to not mix is when you can’t anticipate the animal’s response to pain or changes in the pain state. While it is conceivable to mix butorphanol with another opioid (again dose dependent) if that pain state were to change the tight affinity of butorphanol at the opioid receptor will complicate expected increase in analgesia with the addition of more opioids. There has been some postulation butorphanol and its metabolite hydroxybutorphanol and norbutorphanol may have activity with no analgesic efficacy for up to 8 hours! Essentially, butorphanol and its metabolites are taking up space on the receptor for an extended period of time without the analgesic component. This is certainly true at the kappa receptor respectively. The technique of mixing butorphanol and buprenorphine has been described by many in the general practice setting for spays/neuters. The logic behind this technique is thought to allow butorphanol to express its sedative properties and analgesic properties relatively quickly and as the analgesic properties wanes the buprenorphine should be “kicking in”. Buprenorphine’s time to full efficacy is ~30 minutes with conventional doses used in veterinary medicine, 0.01-0.03mg/kg IV/IM. Subcutaneous administration of any opioid at conventional dosing can dramatically decrease peak effects and plasma levels and is not recommended by the author (Exception, Simbadol label dosing for cats).
However, per receptor theory and various animal and human studies, the idea that buprenorphine exerts no analgesic effects until ~30min if fraught with misunderstanding. Rather, the peak analgesic effects are generally observed around the 30-minute mark after IV, IN, OTM or IM administration of buprenorphine. This is also true for butorphanol and many other opioids. With this understanding the logic behind this technique or with mixing butorphanol with other opioids, like hydromorphone, is flawed and not recommended. Instead, practitioners should consider mixing more reliable opioids with true sedatives/tranquilizers such as acepromazine, dexmedetomidine, gabapentin, trazadone. Butorphanol is best used for shorter, non or minimally painful procedures with other analgesic agents (NSAIDS and local blocks) for a multi-modal approach.
https://pubmed.ncbi.nlm.nih.gov/2165617/
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197734
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7668422/
https://www.frontiersin.org/articles/10.3389/fchem.2020.00335/full
Procedures where butorphanol might be best utilized:
Small laceration repair (with local and NSAID)EndoscopyRhinoscopyMinor tooth extraction (with local and NSAID)Sedated radiographsNail trimsBandage changes (wet-to-dry, casts/splints of broken bones, wounds requiring minor debridement)Download .pdf of this article.